Is an standard format used by health providers to take notes.
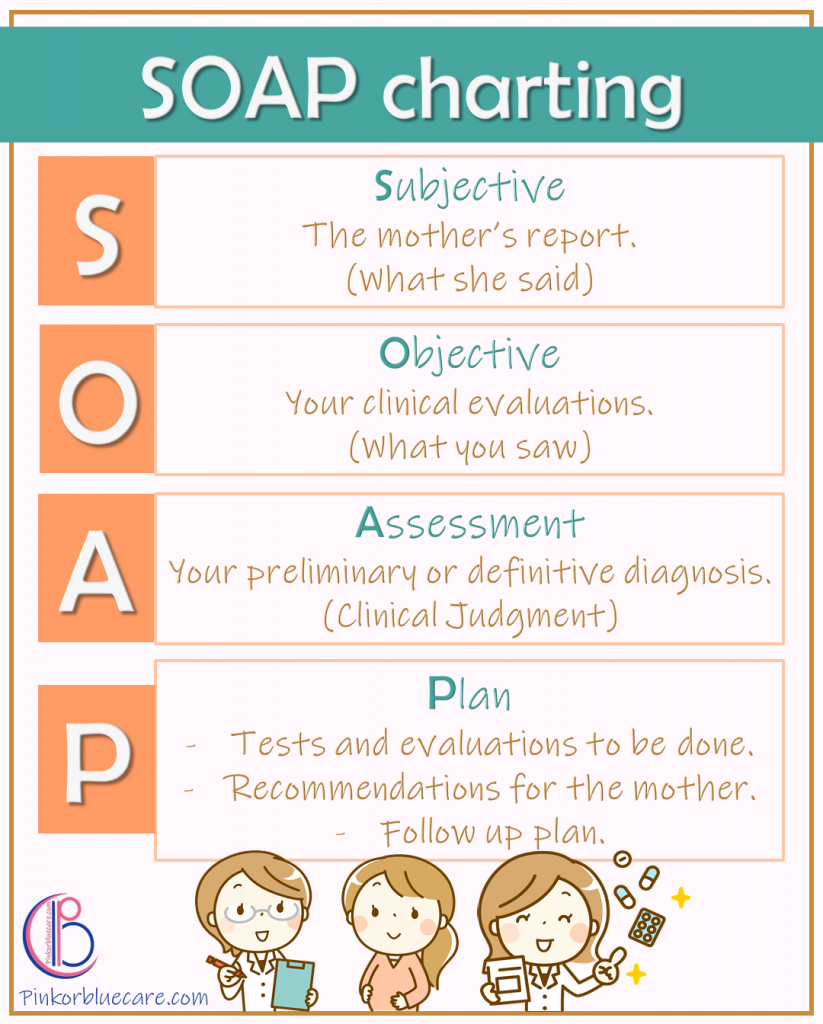
SOAP Charting
Subjective
The mother’s report. (What she said)
Objective
Your clinical evaluations. (What you saw)
Assessment
Your preliminary or definitive diagnosis. (Clinical judgment)
Plan
-Tests and evaluations to be done.
-Recommendations for the mother.
-Follow up plan.
